Spending hundreds on a stool test promising 'personalized' answers? Before you click 'buy,' let's talk about what that expensive report actually tells you.
Your gut microbes play a very important role in the health of the whole body and the gut. If you want to be healthy and live long, it is vital that you take good care of your beneficial microbes. Gut dysbiosis, on the other hand, has been linked to most chronic illnesses, including IBS. Your gut microbes deserve to be noticed!
Home poop tests that measure microbial composition promise that by seeing what microbes there are in your poop, it can help you understand your gut better and give you precise and individualized recommendations to improve gut health.

We all want that silver bullet, but unfortunately, the current science behind these home tests simply doesn't support the marketing claims. Read on to find out the critical reasons why testing your gut microbiome today is premature, and possibly even harmful.
1. The tests are not accurate.
There are multiple different kinds of tests out there, some better than others, but they all have the same issue: they are not accurate. Here are various problems of multiple tests:(a) Some tests only measures bacteria (not fungi/viruses), (b) Functionality is often guessed from diversity, (c) Many microbes go undetected, (d) Contamination with human DNA complicates results.
Also, different tests give different results. Take all the different tests with the same sample and you’ll get different results. This can happen even with testing the same sample with the same test multiple times.
2. Challenges stemming from the microbiota itself
- Your gut microbiome fluctuates even WITHIN A DAY. The relative amounts of different microbes, species and strains are changing constantly. You microbes are different based on the season, your lifestyle, your diet and even the time of day. This means that a test taken in the morning shows a different result than a test taken in the evening. What conclusions can you really draw from this?
- We don’t have a standard with which to compare: science doesn’t know everything about the gut microbiome yet. Including what is ideal, or a healthy gut microbiota. Every person has their own individual microbial fingerprint and we know that diversity is good. But, even IBS doesn’t have an identified microbial signature yet, even though some trends can be detected. If a testing company has a scoring system, it’s not based on sound scientific evidence.
- Correlation does not mean causation: studies can show that in some illnesses, higher numbers of specific bacteria are present. However, this does not prove that those bacteria are what are causing the illness.
Your gut microbiota is highly complex and the truth is that microbiome test results are very difficult to truly interpret, even if they were accurate. This makes providing science-based recommendations based on test results virtually impossible.

Some companies provide dietary recommendations based on the results, however, but the scientific backing to prove them is thin. I contacted a company once to find out how they came up with their "foods to avoid and to eat" lists for different results and they couldn’t provide any real evidence for this.
And what’s worse, making big diet changes and restricting a lot of foods based on these tests can be harmful. They increase malnutrition risk, they increase stress and they can lead to disordered eating and food fears, all of which are damaging to gut health.
Ways to support gut microbe health (evidence-based)
- Lots of diet variety, especially plants
- Feed your gut microbes with fiber and prebiotics
- Fermented foods, potentially probiotics
- Avoid low-quality foods, like certain ultraprocessed foods
- Proper sleep
- Exercise
- Stress reduction
The gut microbiota is hugely important in IBS and in health in general, but testing your poop to see what bacteria it has is not the answer. Rather focus on the foundational lifestyle and diet habits that we know help your gut. It might not be exciting, but it is powerful.
If you need help building these solid lifestyle and diet foundations, join my group program in January 2026! Together we will take 15 gut health steps in 15 days that are designed to take only 15 minutes per day to get through. It’s a low threshold program with no fluff and only evidence-based practices to soothe your digestion. Go here to sign up!
PS. The program has also a version in Finnish, here’s the sign-up page.
References:
Matsuo Y, Komiya S, Yasumizu Y, Yasuoka Y, Mizushima K, Takagi T, Kryukov K, Fukuda A, Morimoto Y, Naito Y, Okada H, Bono H, Nakagawa S, Hirota K. Full-length 16S rRNA gene amplicon analysis of human gut microbiota using MinION™ nanopore sequencing confers species-level resolution. BMC Microbiol. 2021 Jan 26;21(1):35. doi: 10.1186/s12866-021-02094-5. PMID: 33499799; PMCID: PMC7836573.
Wensel CR, Pluznick JL, Salzberg SL, Sears CL. Next-generation sequencing: insights to advance clinical investigations of the microbiome. J Clin Invest. 2022 Apr 1;132(7):e154944. doi: 10.1172/JCI154944. PMID: 35362479; PMCID: PMC8970668.
Heiman ML, Greenway FL. A healthy gastrointestinal microbiome is dependent on dietary diversity. Mol Metab. 2016 Mar 5;5(5):317-320. doi: 10.1016/j.molmet.2016.02.005. PMID: 27110483; PMCID: PMC4837298.
So D, Whelan K, Rossi M, Morrison M, Holtmann G, Kelly JT, Shanahan ER, Staudacher HM, Campbell KL. Dietary fiber intervention on gut microbiota composition in healthy adults: a systematic review and meta-analysis. Am J Clin Nutr. 2018 Jun 1;107(6):965-983. doi: 10.1093/ajcn/nqy041. PMID: 29757343.
Leeuwendaal NK, Stanton C, O'Toole PW, Beresford TP. Fermented Foods, Health and the Gut Microbiome. Nutrients. 2022 Apr 6;14(7):1527. doi: 10.3390/nu14071527. PMID: 35406140; PMCID: PMC9003261.
Pérez-Prieto I, Plaza-Florido A, Ubago-Guisado E, Ortega FB, Altmäe S. Physical activity, sedentary behavior and microbiome: A systematic review and meta-analysis. J Sci Med Sport. 2024 Nov;27(11):793-804. doi: 10.1016/j.jsams.2024.07.003. Epub 2024 Jul 9. PMID: 39048485; PMCID: PMC12510671.
Hantsoo L, Zemel BS. Stress gets into the belly: Early life stress and the gut microbiome. Behav Brain Res. 2021 Sep 24;414:113474. doi: 10.1016/j.bbr.2021.113474. Epub 2021 Jul 16. PMID: 34280457; PMCID: PMC8380711.
Morwani-Mangnani J, Giannos P, Belzer C, Beekman M, Eline Slagboom P, Prokopidis K. Gut microbiome changes due to sleep disruption in older and younger individuals: a case for sarcopenia? Sleep. 2022 Dec 12;45(12):zsac239. doi: 10.1093/sleep/zsac239. PMID: 36183306; PMCID: PMC9742900.
<script type="application/ld+json">
{
"@context": "https://schema.org",
"@type": "BlogPosting",
"mainEntityOfPage": {
"@type": "WebPage",
"@id": "https://www.akwise.co/2025/12/02/microbiome-stool-testing/"
},
"headline": "Microbiome stool testing: why you shouldn’t do them if you have IBS",
"description": "Testing your gut microbes from a stool test are becoming increasingly popular, but are they worth it? Are these tests trustworthy and can they really provide personalized recommendations that ease IBS symptoms?",
"image": "https://www.akwise.co/wp-content/uploads/2025/12/blog-images-poop-testing-2.webp",
"author": {
"@type": "",
"name": "Anna-Kaisa Manolova, RD",
"url": "https://www.akwise.co/anna-kaisa-manolova/"
},
"publisher": {
"@type": "Organization",
"name": "AKWise",
"logo": {
"@type": "ImageObject",
"url": "https://www.akwise.co/wp-content/uploads/2024/11/akwise-logo-grey-xtra-sm-png.webp"
}
},
"datePublished": ""
}
</script>Ever wonder why your poop looks different one day than the other? You probably know what constipation and diarrhea are, but what if the color changes, or your poop looks slimy? Your poop can tell you a lot about your gut health, and in some cases also about your overall health, which is why it’s important to keep an eye on your poop regularly.
Keep reading if you want to find out how to “read” your poop!

Frequency
First, let’s talk about BM frequency, or how often you have a number 2. I consider the ideal to be 1-3 times a day, although officially it’s normal to go less often. In fact, what is normal is slightly different for everyone. Someone might feel great with a bowel movement every 3 days, and for someone not pooping every day is already troublesome.
- If you go less than 3 times per week, this is considered constipation, especially if the stool is pebbly and hard.
- At the other end of the spectrum, diarrhea is thought to be 3 or more loose stools per day, or whatever is abnormal to you.
Consistency
Let’s now take a look at the Bristol stool chart to get a real good visual on what an ideal poop is and what it is not:
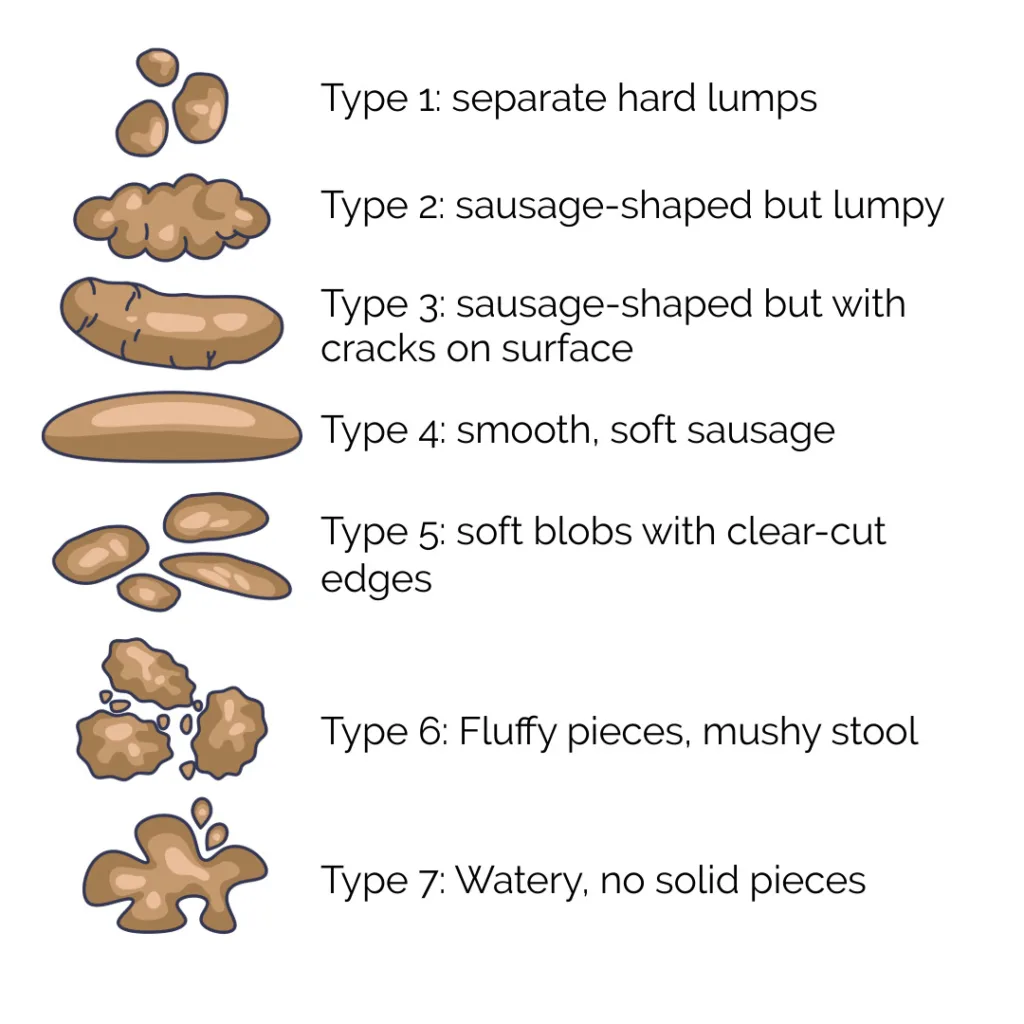
- Types 1 and 2: constipation
- Types 3 and 4: normal
- Types 5-7: diarrhea
Types 1 and 2 are typically the result of not having enough fiber in the diet (fiber makes stools bigger and easier to pass + fiber can make stool softer), not drinking enough fluids (body takes all the moisture it can from stool to prevent dehydration, which makes stool small and hard), or if the stool is moving too slowly through the digestive system, in which case there’s more time for the intestines to absorb water from poop making it hard. If you don’t eat enough fiber, this can slow the passage of stool through also. Stress can also slow your gut motility and cause constipation, and sometimes the cause could be due to pelvic floor muscle problems. Some medications can cause constipation, for example iron supplements. In functional constipation, there is nothing clear to explain it.
To make things a bit more complicated, sometimes constipation can mask itself as diarrhea, for example in the case of overflow diarrhea where a hard stool plug is preventing poop from exiting and only loose stool can get around it to get out.
Food enters the large intestine in a highly liquid form and lots of water needs to be absorbed before the poop is excreted, otherwise we will get dehydrated. Stool types 5-7 indicate a fast passage of stool through the intestines which leaves not enough time to absorb excess fluid from the stool. Or, sometimes intestines can secrete too much water into the intestine, which moves poop through faster and leads to diarrhea.

Infection is the most common cause of diarrhea. Some medications can loosen stools, such as the common diabetes drug metformin, and also food intolerances, like lactose intolerance can do this. Chronic digestive illnesses, like celiac disease, pancreatitis and inflammatory bowel disease are other relatively common, though more severe, causes of diarrhea. Stress can also cause your bowels to empty too fast. A study from this year found a physical mechanism for this, but more on that later.
With IBS, you can have constipation predominant IBS, diarrhea predominant IBS, or a mixed version of the disorder. There’s also IBS-U, IBS unidentified that doesn’t fit well into any of these categories. Let me know if you’d like to understand the difference between each type of IBS and I’ll write a post about it.
Color of poop
Other visual changes in poop can also be signs of problems in the digestive tract. Some of them are serious. See a summary below of the most common poop changes and what they mean.
| Appearance of poop | Meaning |
| Black and tarry | Bleeding in the upper part of the intestine. Blood is partially digested and turns black. However, a more common cause of black and tarry stools are iron supplements, so if you have been taking iron and your poop turns black, not to worry – it’s normal. If not, talk to your doctor! |
| Black (not tarry) | Foods like blueberries, black licorice, blood pancakes, even dark chocolate. Medications like Pepto-bismol, activated charcoal. |
| Red blood | Bleeding in the lower part of the intestines. This is relatively common and often means you have hemorrhoids that got nicked a bit during pooping. If there are streaks of blood on the poop or there’s some blood on the toilet paper after wiping, it could be because of hemorrhoids (or anal fissures) and likely nothing to worry about. If you are concerned, you can doublecheck with your doctor and you can certainly ask how to manage these issues even if the bleeding is not worrysome. If there’s a bigger amount of bright red blood, like if the water in the toilet turns red, then speak with your doctor ASAP. |
| White/clay-colored | Not enough bile. Bile is produced in the liver, stored in the gallbladder and secreted into the small intestine when we eat (fatty) food. It is necessary for digesting fats. The color of bile is yellow-green, but as it moves through the digestive tract, it changes into that typical poop-brown color. If either the liver is not making enough bile, or the gallbladder is unable to squirt bile into the digestive tract, this color will be missing – without bile your poop is light/white. Talk to your doctor if your poop turns white or clay-colored for more than a couple of days. |
| Yellow/orange/green | As mentioned above, the color of poop comes from bile. If intestines move food faster than normal, there’s not as much time for the bile salts to change color. Some antibiotics can turn poop to an orange or green color. Food dyes can color poop as can some foods, like spinach (green) and carrots (orange). |
| Other colors | First think about what you’ve been eating – this is the most common cause of funny colored poop. Food dyes and beetroot can easily give your poop a festive coloration. If there are no other symptoms, like abdominal pain, diarrhea or vomiting, colors you didn’t expect poop to have is likely just related to what you ate. |
| Floaty, unusually stinky, sticky, loose | Fatty stool. This would indicate a problem in the digestion and absorption of fats, perhaps because of a lack of pancreatic enzymes that digest fats, or problems with bile. Celiac disease can damage intestinal villi and cause reduced absorption of fat and can lead to fatty stools also. Contact your doctor if this problem persists. |
| Food pieces in poop | Many fruit, vegetables and seeds have skins that the body just can’t digest and will show up in your poop. This is normal. Eating too quickly and chewing poorly can increase undigested food in poop. Chew your food thoroughly and see what happens. If you have diarrhea, this issue may become more prominent as there’s less time for the digestive enzymes to work. Usually this is nothing to worry about, but if there are other persistent problems, like abdominal pain, weight loss you can’t explain, vomiting etc, please see your doctor. |
| Mucus | Clear mucus is normal, in fact it helps move poop forward in the GI tract. Irritants can cause your GI tract to produce more mucus than usual, like if you have a viral gut infection. White, bloody, or yellow mucus could indicate that something more serious is going on the gut – talk to your doctor. Get checked also, if there are any other symptoms, like abdominal pain, vomiting, weight loss or diarrhea that lasts longer than a few days. |
There are many reasons why your poop may look different sometimes, and usually it’s nothing to worry about. But if the issue persists, and especially if there are other concerning symptoms, it’s important to contact your healthcare provider. I will also add that even if your symptoms are not clearly indicating that there’s something serious going on, but you are feeling very worried about it, it’s not a bad idea to talk to your doctor anyway. Fear and worry cause a stress response, which can worsen symptoms and cause digestive issues, so it’s better to get your symptoms checked than wait and stay worried.
How does your poop look like? If you are not entirely happy with the consistency of it and would like to get those soft banana poops more often, get in touch! I have some tricks up my sleeve to help you.
PS. Do you have bloating and want to reduce it? Download the free ebook “5 Easy Ways to Beat the Bloat” with powerful ways of boosting your digestion to not feel like an inflated balloon by the evening.
References:
Diaz S, Bittar K, Hashmi MF, Mendez MD. Constipation. 2023 Nov 12. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan–. PMID: 30020663.
Nemeth V, Pfleghaar N. Diarrhea. [Updated 2022 Nov 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448082/
DiGregorio AM, Alvey H. Gastrointestinal Bleeding. 2023 Jun 5. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan–. PMID: 30725976.
Azer SA, Sankararaman S. Steatorrhea. 2023 May 16. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan–. PMID: 31082099.
What Does My Stool (Poop) Color Mean? https://my.clevelandclinic.org/health/articles/stool-poop-color Accessed 10/21/2025
Mucus in Stool (Poop). Cleveland Clinic. https://my.clevelandclinic.org/health/symptoms/mucus-in-stool Accessed 10/21/2025
The gluten-free diet has become a booming trend in the recent decade. Many people follow it for perceived health benefits, like reduced inflammation. A gluten-free diet is desperately needed in the treatment of celiac disease, but what about IBS? What about health in general? Despite being trendy, is gluten-free diet a must do for good health?
Is gluten a problem for health?
Numerous studies have looked into gluten and whether restricting it might help different chronic illnesses, including IBS. Unfortunately, at the moment the evidence is clear only for celiac disease. This is the case even for inflammatory bowel diseases. There are not many studies yet, and the results in studies already done have been too variable, and many confounding factors muddle the results, which makes it difficult to say for certain that gluten is a true problem for health and gut health.
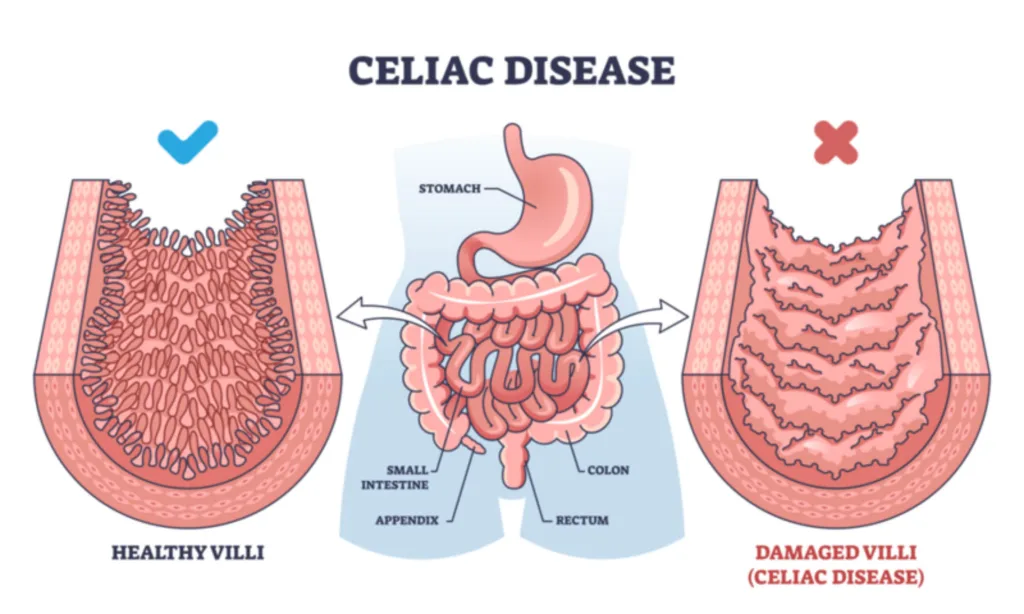
On one hand, there are studies that suggest gluten causes inflammation in the gut. It is certainly known that the severe inflammation from gluten is what causes problems in people with celiac disease and must be avoided.
On the other hand, there are numerous studies showing the anti-inflammatory effects of whole grains. The most common whole grains used in the world contain gluten, and these studies are not specifying that the grains used were gluten-free. Also, the Mediterranean diet, which favors whole grains, is considered to have anti-inflammatory effects.
Thus, it seems that gluten in whole grains does not have the same effect as gluten would on its own. It’s only in celiac disease in which the inflammatory response of the body against gluten is so strong that it overrides the anti-inflammatory effects of whole grains and can clearly be pinpointed as the problem in this illness.
It’s also worth mentioning that studies have not found that gluten causes a higher risk of weight gain, type 2 diabetes or heart disease. In fact, it’s the opposite. Eating gluten through whole grains is associated with lower weight! When the effects of fiber in whole grains are factored into the analysis, gluten on its own is linked to a lower risk of heart disease and type 2 diabetes also. The more gluten, the better it seems. Since type 2 diabetes and heart disease are associated with inflammation, the inflammatory aspect of gluten is all but clear cut.

You’d think that together with celiac disease, non-celiac gluten insensitivity (NCGS) would be an exception. In NCGS, gluten is thought to cause digestive issues without a diagnosis of celiac disease. However, what is interesting, one recent and well-executed study showed that it wasn’t the gluten ingestion, but the expectation that the food had gluten that caused symptoms to appear in people with NCGS in the study. So, if the person believed he was eating gluten, he’d get symptoms regardless of whether the food had gluten in it or not. Only a very small subset of participants seemed to genuinely react to gluten.
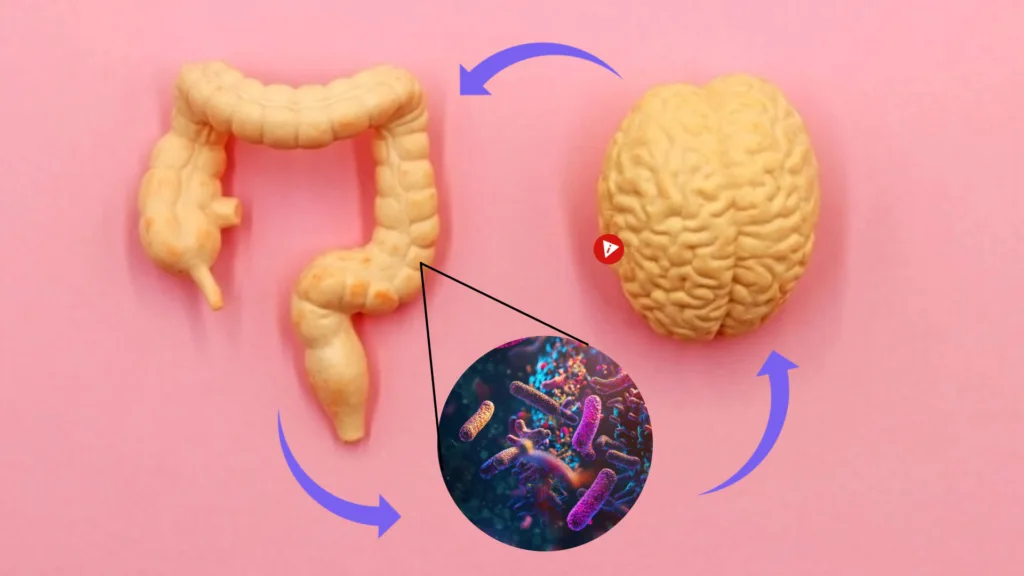
This phenomenon is called the placebo-effect: when you believe something helps you, or harms you, it does. Your brain and gut are intricately connected through the gut-brain axis and your thoughts and expectations have more power than you know.
So, even if it seems like gluten is problematic to you, you need to be very honest with yourself to determine whether it is the placebo effect that is responsible for your symptoms, or if it’s gluten.
Is gluten bad in IBS?
When it comes to IBS, studies have shown that other substances like fructans in gluten-containing foods are the more likely problem than gluten itself. Fructans are a type of FODMAP, which can cause gut symptoms in people who are sensitive to increased gas and/or fluid in the digestive system, which is a typical situation in IBS because of visceral hypersensitivity. Well, should you avoid gluten-containing grains because of the FODMAPs they contain then? Read this blog post to see what I think about FODMAPs.
But if gluten causes inflammation, and a lot of people feel like it causes problems, wouldn’t it be a good idea to avoid it anyway, just in case?
I have bad news for you: following a gluten-free diet might do more harm than good if you don’t have celiac disease.
Risks of a gluten-free diet
- There is evidence that avoiding gluten can be harmful to health. For one, restrictive diets in general are not great for psychological health. Fear of foods is common with restrictive diets and is mentally taxing, and difficulty finding food to eat at restaurants or at social gatherings can feel awkward and stressful. You might start avoiding these kinds of situations, which can lead to loneliness and social isolation. Mental health issues and stress often make digestive problems worse, so restricting your diet in the hopes of improving gut function can end up doing the opposite than what you were hoping for.
- Removing gluten from your diet can cause gut microbiota dysbiosis and change your gut microbiota for the worse, which has negative effects on both gut health and overall health.
- Gluten-free foods are also generally of lower quality as compared to foods that contain gluten, like whole grains. A review study revealed a significant increase in fatty liver disease and metabolic syndrome in people with celiac disease who were on a gluten-free diet and this was attributed to the fact that gluten-free foods tend to have less fiber and more sugar, salt and fat to make up for the lack of gluten. This leads to weight gain and health problems. Of course, not all gluten-containing grains are healthy either, such as packaged and highly processed foods, but whole grains that are not stripped from fiber and micronutrients are of excellent nutritional value.
- According to one study, people on the gluten-free diet had four times higher mercury levels in their body than average.
- There’s some evidence to suggest that gluten stimulates immunity. A small study saw that natural killer cell numbers were higher in the group receiving 3 grams of gluten per day than those who didn’t.

At the end, the big picture about gluten is still not completely clear – more research is needed to clarify all the contradictions. While many studies point to gluten being able to cause inflammation in the gut, it doesn’t necessarily mean that gluten is bad for you. Other studies show how gluten can reduce the risk of heart disease and diabetes, both of which are also linked to inflammation. Weird, isn’t it?
But since following a gluten-free diet is not risk-free, going on the gluten-free diet is probably not useful, and in fact, it can be harmful, if you don’t have celiac disease. If you are considering this as an option, I encourage you to discuss it with an expert so that you don’t end up harming yourself when you are trying to get better.
What I’m most interested in understanding is what are the differences between people who genuinely get symptoms from gluten and those who don’t. Or what happened that you can’t tolerate gluten anymore, even though in the past it was fine. The latter is a question I encourage you to ponder – maybe there’s something that has happened that you can reverse.
Also remember that your health and diet is never about just one nutrient or food. Whether you are healthy or not is a sum of everything you do and eat, and the effect of just one aspect of your diet might not matter as much as you might think.
Thank you for reading! If you know of people who are on the gluten-free diet, or considering it without celiac disease, share this post with them – knowledge empowers you to make informed decisions about your health. That’s why I do what I do.
References
Manza F, Lungaro L, Costanzini A, Caputo F, Volta U, De Giorgio R, Caio G. Gluten and Wheat in Women's Health: Beyond the Gut. Nutrients. 2024 Jan 22;16(2):322. doi: 10.3390/nu16020322. PMID: 38276560; PMCID: PMC10820448.
Skodje GI, Sarna VK, Minelle IH, Rolfsen KL, Muir JG, Gibson PR, Veierød MB, Henriksen C, Lundin KEA. Fructan, Rather Than Gluten, Induces Symptoms in Patients With Self-Reported Non-Celiac Gluten Sensitivity. Gastroenterology. 2018 Feb;154(3):529-539.e2. doi: 10.1053/j.gastro.2017.10.040. Epub 2017 Nov 2. PMID: 29102613.
Iven J, Geeraerts A, Vanuytsel T, Tack J, Van Oudenhove L, Biesiekierski JR. Impact of Acute and Sub-Acute Gluten Exposure on Gastrointestinal Symptoms and Psychological Responses in Non-Coeliac Gluten Sensitivity: A Randomised Crossover Study. United European Gastroenterol J. 2025 Mar 26. doi: 10.1002/ueg2.70014. Epub ahead of print. PMID: 40138597.
Algera JP, Magnusson MK, Öhman L, Störsrud S, Simrén M, Törnblom H. Randomised controlled trial: effects of gluten-free diet on symptoms and the gut microenvironment in irritable bowel syndrome. Aliment Pharmacol Ther. 2022 Nov;56(9):1318-1327. doi: 10.1111/apt.17239. Epub 2022 Sep 29. PMID: 36173041; PMCID: PMC9828804.
Cenni S, Sesenna V, Boiardi G, Casertano M, Russo G, Reginelli A, Esposito S, Strisciuglio C. The Role of Gluten in Gastrointestinal Disorders: A Review. Nutrients. 2023 Mar 27;15(7):1615. doi: 10.3390/nu15071615. PMID: 37049456; PMCID: PMC10096482.
Horiguchi N, Horiguchi H, Suzuki Y. Effect of wheat gluten hydrolysate on the immune system in healthy human subjects. Biosci Biotechnol Biochem. 2005 Dec;69(12):2445-9. doi: 10.1271/bbb.69.2445. PMID: 16377907.
Elli L, Rossi V, Conte D, Ronchi A, Tomba C, Passoni M, Bardella MT, Roncoroni L, Guzzi G. Increased Mercury Levels in Patients with Celiac Disease following a Gluten-Free Regimen. Gastroenterol Res Pract. 2015;2015:953042. doi: 10.1155/2015/953042. Epub 2015 Feb 23. PMID: 25802516; PMCID: PMC4352902.
Sanz Y. Effects of a gluten-free diet on gut microbiota and immune function in healthy adult humans. Gut Microbes. 2010 May-Jun;1(3):135-7. doi: 10.4161/gmic.1.3.11868. Epub 2010 Mar 16. PMID: 21327021; PMCID: PMC3023594.
Lebwohl B, Cao Y, Zong G, Hu FB, Green PHR, Neugut AI, Rimm EB, Sampson L, Dougherty LW, Giovannucci E, Willett WC, Sun Q, Chan AT. Long term gluten consumption in adults without celiac disease and risk of coronary heart disease: prospective cohort study. BMJ. 2017 May 2;357:j1892. doi: 10.1136/bmj.j1892. PMID: 28465308; PMCID: PMC5421459.
Michael D E Potter, Stephen C Brienesse, Marjorie M Walker, Andrew Boyle, Nicholas J Talley, Effect of the gluten‐free diet on cardiovascular risk factors in patients with coeliac disease: A systematic review, Journal of Gastroenterology and Hepatology, 33, 4, (781-791), (2018).https://doi.org/10.1111/jgh.14039
Saturni L, Ferretti G, Bacchetti T. The gluten-free diet: safety and nutritional quality. Nutrients. 2010 Jan;2(1):16-34. doi: 10.3390/nu20100016. Epub 2010 Jan 14. PMID: 22253989; PMCID: PMC3257612.
Mariani P, Viti MG, Montuori M, La Vecchia A, Cipolletta E, Calvani L, Bonamico M. The gluten-free diet: a nutritional risk factor for adolescents with celiac disease? J Pediatr Gastroenterol Nutr. 1998 Nov;27(5):519-23. doi: 10.1097/00005176-199811000-00004. PMID: 9822315.
Valvano M, Longo S, Stefanelli G, Frieri G, Viscido A, Latella G. Celiac Disease, Gluten-Free Diet, and Metabolic and Liver Disorders. Nutrients. 2020 Mar 28;12(4):940. doi: 10.3390/nu12040940. PMID: 32231050; PMCID: PMC7230624.
While incompletely understood, the gut microbiota seems to play an important role in IBS. This, even though an IBS-specific gut microbial signature has not been found. In other words, you can’t tell by looking at someone’s gut microbe test results that they have IBS, but it seems clear that some kind of imbalance in the composition of gut microbes is often present in IBS.
For this reason, impacting the gut microbiota through probiotics has been a hot research topic recent years.

What are probiotics and are they helpful or IBS?
Probiotics are live micro-organisms that have a health promoting effect on us. Lots of research has been done on IBS and probiotics, yet the studies have been very different from each other, which makes it difficult to compare these studies and make firm conclusions and recommendations. This is why national IBS guidelines are usually quite vague about their recommendations. The American College of Gastroenterology doesn’t recommend them at all at this point, while other national guidelines are more neutral – they say probiotics may help but it’s not clear which probiotic is best for which symptom.
Many probiotic products certainly claim to ease IBS symptoms by improving the microbial balance in the large intestine. On top of this, I know of many cases in which simply starting a probiotic made symptoms nearly disappear.
So, are probiotics a silver bullet for IBS? The truth is, It’s not clear. In my experience, they could help some people, but not all. It seems to be a highly individual matter that depends on many factors and at the moment there’s no way of knowing in advance who might benefit and who might not.

Thinking about trying probiotics to ease IBS symptoms?
Here are a few points to be aware of:
- It matters what you choose. Pick a specific species and even strain.Do some research – pick one that is studied for the symptom(s) your are trying to relieve. Pay attention if the product should be a single strain probiotic, or an assortment of a few. I can help you if you aren’t sure where to look.
- Try the probiotic for at least 4 weeks to see if there’s a benefit. If nothing happens in this timeframe, there’s no use continuing it.
- Probiotics can’t colonize the gut, which is good and bad. It’s good in that if the probiotic doesn’t work for you and even makes your symptoms worse, then the offending strain will leave your system soon enough. But bad in that you have to keep taking the probiotic to benefit from it. This can be expensive in the long run.
- Your symptoms might get worse for a few days on a new probiotic. This is normal, so be patient. If after a week things are not improving/normalizing, stop taking the probiotic.
- Probiotic products vary hugely in quality and purity. Always choose a product that has a third-party verification. Otherwise, you have no idea if the product has the bacteria it’s supposed to have, and only that. Many products might be contaminated with ingredients and bacteria that shouldn’t be there, and sometimes this can be dangerous. Thankfully, in Europe probiotic products are much more regulated than in the US, which makes finding a reputable one easier.
- Make sure the product has enough of the bacterial strain you need. If the dose is too low, it won’t likely have the desired effect.
- With high quality products, the risk of using probiotics is low – there is virtually no harm in trying them, unless you have problems with low immunity (like from cancer treatments). Small intestinal bacterial overgrowth is another diagnosis for which I wouldn’t recommend probiotics. If you are pregnant or breastfeeding, check with your doctor to make sure it’s safe for you.
- Store probiotics carefully. Live organisms can die if it gets too cold or too hot. They also lose potency over time.
Probiotics for IBS? What’s the conclusion?
Should you try probiotics? To me, probiotics could be helpful for IBS, but there are still many unknowns about them. They may help some, but it seems to me that there are other therapies that are probably more useful to invest in first, such as calming the gut-brain axis, the interaction problem between the gut and the brain. Methods that do this calm your nervous system and reduce stress, and as a bonus, they support gut microbes, too.
Need tips? Here’s an idea, or give me a call and we can chat about your options.
PS. Are you struggling with bloating? If yes, you might benefit from my free ebook “Why the Balloon Belly”, download it here.
References
Hillestad EMR, van der Meeren A, Nagaraja BH, Bjørsvik BR, Haleem N, Benitez-Paez A, Sanz Y, Hausken T, Lied GA, Lundervold A, Berentsen B. Gut bless you: The microbiota-gut-brain axis in irritable bowel syndrome. World J Gastroenterol. 2022 Jan 28;28(4):412-431. doi: 10.3748/wjg.v28.i4.412. PMID: 35125827; PMCID: PMC8790555.
Merenstein D, Pot B, Leyer G, Ouwehand AC, Preidis GA, Elkins CA, Hill C, Lewis ZT, Shane AL, Zmora N, Petrova MI, Collado MC, Morelli L, Montoya GA, Szajewska H, Tancredi DJ, Sanders ME. Emerging issues in probiotic safety: 2023 perspectives. Gut Microbes. 2023 Jan-Dec;15(1):2185034. doi: 10.1080/19490976.2023.2185034. PMID: 36919522; PMCID: PMC10026873.
Satish Kumar L, Pugalenthi LS, Ahmad M, Reddy S, Barkhane Z, Elmadi J. Probiotics in Irritable Bowel Syndrome: A Review of Their Therapeutic Role. Cureus. 2022 Apr 18;14(4):e24240. doi: 10.7759/cureus.24240. PMID: 35602835; PMCID: PMC9116469.
For a long time, depression has been thought to be a combination of genetic susceptibility and environmental factors. Only recently experts have begun to realize that another factor is at play – the gut-brain axis.
So far, I’ve focused on the gut-brain axis from the digestive symptoms and IBS point of view, here for example. This time I’d like to bring up gut-brain axis from the brain side of things and talk about how it’s linked with depression.

What is depression
Depression is the most common mental illness in the world. Millions of people are affected by it. We all know how it feels like when you just don’t feel like doing anything, you feel anxious, low in energy and can’t sleep well. When it’s depression, imagine feeling this way for long periods of time.
It’s hopeful that scientific research continues to unearth the mechanics of depression better and better. No longer are medications the only way to improve depressive symptoms. You can support your mental wellbeing through the gut-brain axis, which is accessible through everyday actions!
How does the gut-brain axis influence depression? This is not completely understood yet, but it looks to have a lot to do with your gut microbiota. For one, the gut-brain axis is a two-way communication pathway between the gut and the brain and for two, your gut microbes can tap into this communication and send signals to the brain. The trillions of gut microbes we all have in our large intestines have a tremendous effect on our mood!
Studies looking at the gut microbiota of people with depression are showing noticeable negative changes in microbial composition and diversity. This is problematic, because all the different microbes have slightly different functions in the gut through the variety of substances, like short chain fatty acids and signaling molecules they make. In very simple terms, some of these substances can reduce inflammation, and some of them can promote inflammation. Inflammation in the long term is harmful not just for the gut, but also for the brain. Negative changes in gut microbiota composition leads to an increase in inflammatory substances.
And now, the big question: how can you positively impact your gut microbes to lower the risk of depression, and to perhaps even reduce depressive symptoms?
Two instant tips for fighting depression
1.Eat at least 30 different plant foods every week. When your diet is very varied, your healthy gut microbes get a great array of nutrients and different fibers that allow them to thrive. With many food sources available to them, a higher variety of different species and strains can live in your large intestine and produce all the anti-inflammatory substances that help your brain.
It’s easier than you might think! Begin to vary your breakfast cereal type, your salad ingredients and mix it up with roasted veggies. Add different kinds of seeds and nuts into your oatmeal or eat as a snack, and be sure to add in some beans or lentils every week, too. Mix it up with the fruits you eat every day, and use spices in cooking – soon you will notice you can easily eat more than 30 different plant foods a week.

2.Avoid processed grains and choose whole grains. Whole grains are rich in fiber, and fiber feeds your good gut bacteria. White bread, pasta and rice are all made from processed grain of which the fiber and most other nutrients are removed, leaving behind mostly starch. Tasty for sure, but not nutritious. Instead, choose less processed whole grains, like whole grain bread and pasta and brown rice. You’ll also feel fuller longer. You can check if a food is whole grain by simply reading the ingredients list – if whole grain is mentioned first, then it’s a fiber-rich choice.
The great thing about these small changes is that you will probably notice changes not only in your mood, but in many other ways as well. Time and again we see how in the body everything affected by everything. I’m excited to see your health improve!

Love,
Anna-Kaisa
PS. Would you like to have a quick free consult with me to see where you are at with your gut health? Go here to book.
PPS. A brand new Ebook has just been released! If you are suffering from bloating that is getting in the way of daily life and you would like to understand what is causing it, download it here!
References:
Chang L, Wei Y, Hashimoto K. Brain-gut-microbiota axis in depression: A historical overview and future directions. Brain Res Bull. 2022 May;182:44-56. doi: 10.1016/j.brainresbull.2022.02.004. Epub 2022 Feb 11. PMID: 35151796.
Reyes-Martínez S, Segura-Real L, Gómez-García AP, Tesoro-Cruz E, Constantino-Jonapa LA, Amedei A, Aguirre-García MM. Neuroinflammation, Microbiota-Gut-Brain Axis, and Depression: The Vicious Circle. J Integr Neurosci. 2023 May 8;22(3):65. doi: 10.31083/j.jin2203065. PMID: 37258450.
McDonald D, Hyde E, Debelius JW, Morton JT, Gonzalez A, Ackermann G, Aksenov AA, Behsaz B, Brennan C, Chen Y, DeRight Goldasich L, Dorrestein PC, Dunn RR, Fahimipour AK, Gaffney J, Gilbert JA, Gogul G, Green JL, Hugenholtz P, Humphrey G, Huttenhower C, Jackson MA, Janssen S, Jeste DV, Jiang L, Kelley ST, Knights D, Kosciolek T, Ladau J, Leach J, Marotz C, Meleshko D, Melnik AV, Metcalf JL, Mohimani H, Montassier E, Navas-Molina J, Nguyen TT, Peddada S, Pevzner P, Pollard KS, Rahnavard G, Robbins-Pianka A, Sangwan N, Shorenstein J, Smarr L, Song SJ, Spector T, Swafford AD, Thackray VG, Thompson LR, Tripathi A, Vázquez-Baeza Y, Vrbanac A, Wischmeyer P, Wolfe E, Zhu Q; American Gut Consortium; Knight R. American Gut: an Open Platform for Citizen Science Microbiome Research. mSystems. 2018 May 15;3(3):e00031-18. doi: 10.1128/mSystems.00031-18. PMID: 29795809; PMCID: PMC5954204.
If you have IBS, doesn’t matter which subtype you have, you have undoubtedly been thinking about the foods that you shouldn’t be eating. The ones that might cause or worsen your IBS symptoms.
Because food is the thing that you put into your stomach and intestines and for this reason it must be playing the most important role in how your symptoms happen.
Food does matter. But it’s not in the way that you would necessarily expect! (And it’s not the only thing that matters, but that’s a discussion for another blog post.)

If I asked anyone with IBS on the street what they shouldn’t eat, the answer most likely would have a lot to do with FODMAPs. They might mention onion, garlic or wheat, or some other food that is high in FODMAPs. FODMAPs are small prebiotic fibers that you can’t digest, but your gut microbes can. This microbial fermentation of FODMAPs in the large intestine is what leads to gut symptoms in people with IBS (and in people without IBS, although gut symptoms not as readily).
Unfortunately, the story about FODMAPs in IBS is a more complicated one than this. Yes, the low FODMAP diet has been researched and looks to improve IBS symptoms at least a little in up to 2/3 of patients with IBS. But FODMAPs do not cause IBS. On the contrary, they are beneficial for your digestive health as they are food for your friendly gut bacteria that keep you healthy.
If you eliminate all FODMAPs from your diet, you will change your gut microbiota balance for the worse. You should always include some FODMAPs in your diet. Read more about the low FODMAP diet here. Do not jump into the diet without talking to an expert first.
What you shouldn’t eat is not about FODMAPs
Here’s the big reveal: what I would say you shouldn’t eat if you have IBS is a Western diet. You know, the kind that consists of burgers, hot dogs, sweets, chips and sodas, and not much, if any, fruit, vegetables or whole grains.
I’m sure you have some idea about why a Western diet is not good for you or your gut, but there are many reasons why it’s especially bad if you have IBS.

Why the Western diet makes IBS worse
Four reasons why a Western-style eating pattern is detrimental for digestive health:
- Lack of essential nutrients. Your body, including your digestive system, needs certain nutrients every day to function well. All the bodily tissues and the metabolic reactions within each body cell requires energy, protein, essential fatty acids and vitamins and minerals to do their job. For example, zinc is needed in hundreds of ways in the body, and essential fatty acids become parts of the membranes that envelope each and every body cell. In the gut, some nutrients take care of the gut barrier, helping to make sure that harmful substances can’t cross into the blood stream to cause you problems.
- Lack of fiber. Fiber not only keeps your intestines working regularly, but it is also very important for your gut microbiota. The microbes in your gut can keep you healthy if you give them food every day. If not, they may begin to harm your health – such as your brain, your heart, your liver and of course, your digestion. Good gut bacteria make vitamins and many other types of molecules that help us, but they can’t do this if they don’t have food. Without fiber, microbial diversity suffers, and with this its function. Fiber is also needed to keep your gut barrier working as it should.
- Lack of antioxidants. Antioxidants, like polyphenols, protect your body from damage and can reduce inflammation. Polyphenols are also food for your good gut microbes.
- Too much fat, especially saturated fat. Fat in excess is difficult for your digestion. It can harm your intestines' topmost cell layer, which can cause things to pass into your bloodstream that shouldn't. This also can harm your gut microbiota. Even worse if you don't have a lot of fiber in your diet.
- Additives. Western-type diet is usually very high in packaged and processed foods, which means that very likely they also contain a lot of additives, like preservatives, emulsifiers, and other substances that prolong shelf life of the product and make the texture or taste more desirable. A lot of these additives can be harmful for your digestion.
These five points lead to three ways in which Western diet can harm your digestive system: inflammation, gut microbiota dysbiosis and increased intestinal permeability. Let’s now take look at them.
Inflammation and increased gut permeability
Inflammation: all these points above can cause inflammation in the intestines. On top of this, people eating lots of calorie-rich yet nutrient-poor foods tend to gain weight, which also has an inflammation promoting effect. While IBS is not caused by active inflammation in the intestines, a low level of inflammation can contribute to IBS. Inflammation is caused by your own immune system and is a necessary function of the body, but when inflammation sticks around longer, it can lead to hypersensitivity of the intestines and many other problems.
Microbial dysbiosis: your large intestine is a home of trillions of bacteria, viruses and yeasts. Many of them are beneficial to health by producing vitamins and substances that reduce inflammation, like short chain fatty acids. You also have illness-causing bacteria in your gut, which is not a problem as long as there is a good balance (eubiosis) of all the microbes in your gut. When the balance becomes broken (dysbiosis), harmful bacteria begin to thrive, which can lead to inflammation and increased gut permeability.
Increased permeability: your gut is very good at absorbing valuable nutrients through the gut wall into the blood stream and leaving out harmful substances and bacteria. When something, like a low quality diet, harms permeability, harmful substances have a better chance of getting through into the blood stream. Since now they can travel anywhere in the body, they can cause problems, like inflammation, anywhere in the body too.
These three gut harming factors are also mechanisms that are thought to cause IBS symptoms. This can lead to discomfort or pain, and slower or faster than desired intestinal motility, or in other words diarrhea or constipation. Your gut-brain axis is a major player in IBS and while it isn’t directly affected by food, it is certainly very much affected by your gut microbiota and inflammation. And as you now know, diet affects your gut microbes and inflammation a great deal.

What to do instead
Instead of the Western diet, I recommend eating a Mediterranean-type diet. Research repeatedly shows that the Mediterranean diet benefits us in pretty much every way, from living longer to weight loss and diabetes. It helps reduce inflammation and keeps both your gut microbes and gut barrier in good shape.
The Mediterranean diet is characterized by high intake of fruits, vegetables, legumes, nuts, olive oil, and fish, and low consumption of red meat, dairy products, and saturated fats. Use it as a template on which to build your own individualized gut-healthy IBS diet.
But what about FODMAPs? Why is this diet a thing in IBS if FODMAPs are good for you? The thing is, FODMAPs don't really cause IBS symptoms, even though it might seem like it. The real problem is that your gut is more sensitive to everything going on in there, and since FODMAPs tend to increase gas, a sensitive gut can feel this as discomfort when normally it wouldn’t necessarily be felt at all. So, it’s the hypersensitivity that is the problem, and that’s a more effective target for IBS than simply removing foods from your diet. This is where calming the gut-brain axis comes in.
Calming your gut-brain axis is my aim with each of my online programs, and when working with clients 1-on-1 – I’ve seen great results! I look at everything that is going in your life that could be messing with your gut-brain axis and IBS symptoms, including diet, stress and sleep. If you’d like to explore what working with me might look like, book a free 30-minute call with me today.
Thank you so much for reading! I hope this helps 🙂

Much love,
Anna-Kaisa
Registered Dietitian
IBS and gut-health expert
AKWise.co
PS. Are you struggling with bloating and not sure what is causing it? I have a brand new free Ebook in which I explore more than 10 gut illnesses that cause bloating and provide every day remedies that have the power to ease bloating no matter what is causing it. Want it? Go here.
References:
- García-Montero C, Fraile-Martínez O, Gómez-Lahoz AM, Pekarek L, Castellanos AJ, Noguerales-Fraguas F, Coca S, Guijarro LG, García-Honduvilla N, Asúnsolo A, Sanchez-Trujillo L, Lahera G, Bujan J, Monserrat J, Álvarez-Mon M, Álvarez-Mon MA, Ortega MA. Nutritional Components in Western Diet Versus Mediterranean Diet at the Gut Microbiota-Immune System Interplay. Implications for Health and Disease. Nutrients. 2021 Feb 22;13(2):699. doi: 10.3390/nu13020699. PMID: 33671569; PMCID: PMC7927055.
- Malesza IJ, Malesza M, Walkowiak J, Mussin N, Walkowiak D, Aringazina R, Bartkowiak-Wieczorek J, Mądry E. High-Fat, Western-Style Diet, Systemic Inflammation, and Gut Microbiota: A Narrative Review. Cells. 2021 Nov 14;10(11):3164. doi: 10.3390/cells10113164. PMID: 34831387; PMCID: PMC8619527.
- Barber TM, Kabisch S, Pfeiffer AFH, Weickert MO. The Effects of the Mediterranean Diet on Health and Gut Microbiota. Nutrients. 2023 Apr 29;15(9):2150. doi: 10.3390/nu15092150. PMID: 37432307; PMCID: PMC10180651.
- Beam A, Clinger E, Hao L. Effect of Diet and Dietary Components on the Composition of the Gut Microbiota. Nutrients. 2021 Aug 15;13(8):2795. doi: 10.3390/nu13082795. PMID: 34444955; PMCID: PMC8398149.
- Berding K, Vlckova K, Marx W, Schellekens H, Stanton C, Clarke G, Jacka F, Dinan TG, Cryan JF. Diet and the Microbiota-Gut-Brain Axis: Sowing the Seeds of Good Mental Health. Adv Nutr. 2021 Jul 30;12(4):1239-1285. doi: 10.1093/advances/nmaa181. PMID: 33693453; PMCID: PMC8321864.
You've probably noticed that I often talk about stress and the gut-brain axis. It's a recurring theme here on the blog and on my social media, and even though I’m risking sounding like a broken record, it's for good reason.
Through these discussions, many of you have shared a common experience: feeling significantly more bloated on workdays compared to your days off. It's fantastic that you've been able to connect this to the information I've shared about the link between bloating and stress.
Indeed, stress is a probably the biggest culprit in why you might experience bloating specifically on workdays. Stress can influence how fast your intestines move food and gas, which can lead to gas build-up and discomfort. Stress can also cause irregular contractions and relaxation of your abdominal muscles, causing a puffed up look. Lastly, stress can heighten the sensitivity of your gut. This means that on workdays, your gut may react more strongly to normal digestive processes, such as the presence of food, leading to feelings of discomfort and fullness. On your days off, when you're more relaxed, your gut might not even register these same sensations. This phenomenon is known as visceral hypersensitivity and it’s likely that your IBS might know it all too well too.

Beyond stress, other factors in your workday routine could be contributing to bloating. Here are four additional possibilities:
- Speed Eater Extraordinaire: Is your lunch break looking more like a pit stop? When you're "inhaling" your food in a hurry, you swallow a ton of extra air. Plus, when you feel rushed, your gut feels it too! And I bet you don’t end up chewing your food down enough to support your digestion. Those bigger chunks of food are hard to digest, leading to bloating.
- The Feast or Famine Rollercoaster: Whether it's skipping meals due to lack of time or grazing on small amounts of food throughout the day, both of these eating patterns can disrupt your digestive system's natural rhythm, potentially leading to bloating.
- Desk Jockey Blues: Let's be honest, most of us are glued to our chairs at work, which isn't your bloated belly's best friend. Sitting for long stretches can trap gas and make you feel like you've swallowed a balloon (and maybe even look like it!). You might even get gas pains from big gas bubbles that are desperately trying to find their way out.
- The Processed Food Parade: When time is tight, those ready-made meals and processed snacks can seem like a lifesaver. But sometimes, our guts just aren't fans of all the extra ingredients and preservatives. They can be harder to digest than those lovingly prepared meals you make at home.
So, what can you do to minimize workday bloating?
You guessed it - do the opposite to what you feel is the problem.
⭐ See if you could batch cook meals to take to work instead of relying on ready-made meals. If this is too much, don’t worry too much about it, I always recommend against thinking that your food is unhealthy or bad for you. Give yourself a break – ready-made meals are fine if that’s what you need to do. Eating food is better than skipping meals!
⭐This brings us to the importance of regular meals, ideally every four hours or so. This timeframe allows your stomach to finish digesting the previous meal before more food is introduced - having to mix newly eaten food with partially digested food is not ideal! You're also less likely to be ravenous, which can lead to eating a lot of food quickly.

⭐ Explore ways to dedicate more time to your meals during the workday. Could you block out time in your calendar or discuss a slightly longer meal break with your supervisor? Think about your specific circumstances and creatively think of potential solutions. If there’s nothing you can do about the length of your meal break, at least cultivate a sense of calmness when you eat. Imagine that there’s no rush. Chew your food thoroughly, almost to a puree. Sip water with your meal, avoiding large gulps, and ideally, avoid ice cold drinks.
⭐ Make an effort to take breaks from sitting every hour. A brief walk around the office, a short stroll outside, or even just walking in place next to your desk are great. Some gentle stretches or a yoga pose can also get the gases in your gut moving.
⭐ Regarding work-related stress, explore potential solutions such as discussing your workload and tasks with your supervisor to make sure you have everything you need and aren't feeling overwhelmed. If a workload overhaul isn't in the cards, see if you can change the way you respond to your work tasks. Cultivate a sense of confidence that you’ll get everything done in time. Every time you feel stress lurking behind your back ready to take over, stop for a bit to take a few deep breaths, or take a few minutes to do a breathing exercise. Breathing exercises are excellent as a stress release routine also even when you don’t feel stress – pick a time in your day, like bedtime, to spend a few minutes practicing. When you calm your nervous system regularly, unconscious stress melts away and you can avoid getting stressed out as often.
Don’t know any breathing exercises? Here’s a very powerful one from my facebook page.

Have you noticed this workday-bloat phenomenon yourself? I'd love to hear about your experiences and what you've found helpful in managing it. Email me at [email protected], use this contact form, or just leave a comment below!
But listen, if this bloating is becoming a real problem and affecting your daily life, it's definitely worth taking a closer look. That's why I've created my brand new FREE Ebook: "Why the Balloon Belly?".
Inside, you'll find a practical table outlining more than ten potential causes of bloating, which can help you compare your symptoms to different gut-related issues. If anything in there resonates with you, it might be a good idea to connect with your doctor or me to discuss the next steps and whether further investigation is warranted.
Ready to explore the potential reasons behind your discomfort? You can download the free Ebook here.
While bloating is a common experience, and some bloating is completely normal for a well-working digestive system, persistent discomfort doesn't have to be something you simply accept. Understanding the possible underlying problem is the first step towards feeling better and regaining control. I hope this post has been a helpful starting point.

Love,
Anna-Kaisa
If you thought the answer is “the low FODMAP diet”, you wouldn’t be the only one. Sadly, it’s not as simple as you might expect.
As a dietitian, I’ve taken care of a lot of different kinds of people with all kinds of health problems. Everyone is an individual and diet must always be individualized, but it seems that IBS is much more difficult to generalize than other health problems.
For example, if you have diabetes, you should always pay attention to everything that affects your blood sugar levels. Most often this means counting all the carbohydrates you eat, and sometimes also taking protein and fat into account. For cardiovascular disease, fat quality is something that everyone with high cholesterol needs to consider.

When it comes to IBS, there is no “one-size-fits-all” diet that works for everyone. For one, there are four different IBS types and the advice you give to someone with diarrhea is not the same if the problem is constipation instead.
While the low FODMAP diet is the most “popular” diet for IBS, in my expert opinion, the low FODMAP diet is overused and is NOT a good idea for many, if not most, people. You can read why in my two blog posts “Is the low FODMAP diet the best diet for IBS?” and “Should you try the low FODMAP diet for IBS?”. I know most other dietitians love the low FODMAP diet, but I can’t overlook all the problems that come with this diet. Yes, FODMAPs are small fibers that are easily fermented by your gut microbes and cause relatively more gas, but this happens in everyone, not just in people with IBS. The reason why you are more sensitive to them is because of visceral hypersensitivity, which is caused by IBS (this sensitivity is something I want to improve, rather than just remove foods as a bandaid solution).
So, if it’s not the low FODMAP diet, then what is the right diet for IBS?
It certainly is a highly individualized one. Here are the first five diet and food related questions you should ask yourself regardless of your IBS symptoms:
- How often do I eat?
- How big are my meals?
- How quickly do I eat?
- Do I chew my food until it’s apple sauce consistency?
- What’s my frame of mind when I eat?

I find that regular eating times, and not eating too often or too seldom, lay a foundation for a gut healthy diet. This way you are less likely to overeat or keep taxing your digestion with new food all the time. Eating too quickly results in food that is poorly chewed and a belly full of air, both of which cause bloating and indigestion. Chewing properly begins the digestive process right away and makes food more digestible. Eating when stressed, worried or angry triggers a stress response, i.e. the body’s fight-or-flight mode, which is terrible for digestion. The fight-or-flight mode is the opposite from the rest-and-digest mode. To harness the digestion-promoting rest-and-digest mode, make sure to eat when you feel calm, find a calm environment, and sit down.
Some clients of mine have found that this is all they need to keep their symptoms at bay! So, while they seem simple, these points are truly foundational and have an enormous effect on how well you digest and absorb your food.
What else for IBS?
Once the foundation is well in place, it’s important to find out if your diet is in balance, especially thinking of your individual symptoms. Balance means getting all the nutrients your body needs to be well while including food items that support easing your symptoms, and it also means that your microbiota gets all the food they need. Your gut microbes keep you well if you nourish them properly. Well-fed beneficial bacteria then send positive signals to the brain through the gut-brain axis, with health promoting effects.

A balanced diet is an optimal mix of protein, fat, and carbohydrates (including fiber), as well as vitamins, minerals and antioxidants. A plate method is a nice way of visualizing a balanced diet (see image above), but this also is a generalization that is not appropriate for everyone. It also doesn’t address fat in the diet.
What’s more, sometimes it’s not your diet that is the problem – there are situations when it doesn’t matter what you eat and your symptoms are difficult anyway. This is because IBS is caused by a problem in the way in which your gut and your brain talk to each other, and food is not exactly what causes this disruption. I talk about the gut-brain axis in a blogpost here, a great read!
Are your eating habits helping you ease IBS symptoms? Is your diet in balance?
If you are not sure, get in touch with me. During a 30-minute free gut health review I will give you the tools to build a diet that will keep your gut, and the rest of your body happy, but not only that. We’ll address your gut-brain axis also, for best results. Book your free call here.

Love,
Anna-Kaisa
PS. Don’t wait to get individualized advice for FREE! Book your call now.
PPS. Did you download my free Ebook “5 Easy Ways to Beat the Bloat” yet? These five ways are simple, yet effective in easing bloating that you can put to use right away.
I was at a networking lunch where the lady next to me, after hearing that I specialize in IBS and gut health, started talking to me about her experience on using Ozempic. You’ve heard of Ozempic, right? With the help of this drug, she lost 25 kg (55 lbs) in a year, but as a “side effect” her long term digestive issues were greatly improved.
Fascinating! I had heard about this in passing before, so I wanted to take a deeper look into the drug and whether this is a proven effect.
But first, what is Ozempic?
Ozempic is a brand name for the drug semaglutide, a prescription medication to help people with type 2 diabetes to better control their blood sugar levels, and more recently to help people lose weight. Blood sugar becomes lowered through the hormone insulin, which is released into the blood stream in larger amounts, and weight loss is becomes possible through lowered appetite. It’s also likely that eating sugary and fatty foods (and drinking alcohol) becomes less rewarding, leading to weight loss. (2)
Ozempic is a once weekly injection, and it acts as a GLP-1 agonist. This means that the drug mimics the action of the gut hormone GLP-1 (1). And here’s what explains the gut side effects: as a gut hormone it also helps regulate digestion – it decreases stomach movements and secretions, and slows down digestion.
Interestingly, L-cells that secrete GLP-1 in the gut have different functions depending on their location. In the small intestine, GLP-1 is released in response to nutrients (food) in the GI tract, but further down in the large intestine these cells become stimulated by bile acids, fiber, short chain fatty acids and gut microbes. In the same way, GLP-1 seems to slow things down higher in the intestines and speed things up lower down (5), although some studies suggest that also the large intestine becomes slower. GLP-1 has also been found to improve increased permeability in the large intestine, though the study was done in rats (6).

Ozempic digestive side effects
While the lady I talked to mentioned improvements in her gut issues, interestingly the most common side effects are digestive problems: nausea, constipation, diarrhea, abdominal pain and heartburn. (1) Furthermore, even more severe gut problems can be caused by Ozempic and the like - the risk of pancreatitis, stomach paralysis, bile issues and gut obstruction are increased. It’s not clear why this happens, but it probably has something to do with the ability of GLP-1 agonists to slow down the movements of the digestive tract. (3,6)
When it comes to IBS specifically, some evidence shows that GLP-1 levels are lower in people with constipation predominant IBS and these lower levels are connected also with abdominal pain. However, in a study with mice with something like IBS-C, GLP-1 levels where higher than in normal mice. (4)
Importantly, GLP-1 can worsen stress-related changes in intestinal motility and stimulate the HPA-axis (of which the end products are stress hormones). This is bad news, as stress is recognized as a major trigger of IBS. At the same time, GLP-1 may reduce abdominal pain. (4)

What does this all mean?
This all sounds a bit confusing, so what should you think about this all?
GLP-1 is certainly an important gut hormone that all of us have naturally, but medications that mimic this hormone to boost its function are not unproblematic. And while GLP-1 agonists act on the gastrointestinal tract, scientists are only beginning to explore whether they could be utilized as an IBS therapy at some point in the future. If you are someone who is considering, or already on Ozempic or something like it, please keep the severe gut side effects in mind, so that if your gut function changes drastically, or new symptoms arise, you get them checked out immediately.
Since supportive diet and lifestyle changes are necessary (and based on what the lady told me, often forgotten) even when on this medication, this is a factor to consider and maximize first. If you are not sure what this means, you can write to me.
Also, you can begin supporting your GLP-1 levels naturally by choosing foods that stimulate GLP-1 secretion, like eggs, avocado, olive oil, nuts, and high fiber foods (whole grains, vegetables) (7-12). There’s also some evidence that certain probiotics can enhance GLP-1 secretion, for example Akkermansia municiphila (12).

Get your doc to give you the full story
Many medications have side effects that affect the digestive system. Whether GLP-1 agonists are helpful or harmful depends on the individual. Importantly, talk with your doctor about the GI side effects to make sure the drug is suitable for you. If you are feeling confused, or unsure, ask follow up questions. In fact, any time you are at the doctor’s office and have questions, voice them out! Too often I hear people being disappointed with their doctors leaving them confused about what they should do, especially when it comes to IBS, so demand more detailed explanations. This is your health that we are talking about at the end of the day and it’s the doctors job to explain to you properly.
Thank you so much for reading about this timely topic! Be in touch if you have questions, or if you’d like a topic to be discussed here ([email protected]).

Love,
Anna-Kaisa
PS. Did you download my free ebook yet? Get it here.
PPS. Learn to Meditate –course 2.0 is starting in 3 weeks! If you want a method that gets better at mending your gut-brain axis with time (the root cause of IBS), this course is excellent for you. Sign up here - only $105!
References:
- Puckey, M. Ozempic. Drugs.com. 2025. https://www.drugs.com/ozempic.html accessed 3/6/2025
- Smith NK, Hackett TA, Galli A, Flynn CR. GLP-1: Molecular mechanisms and outcomes of a complex signaling system. Neurochem Int. 2019 Sep;128:94-105. doi: 10.1016/j.neuint.2019.04.010. Epub 2019 Apr 17. PMID: 31002893; PMCID: PMC7081944.
- Dewan, P. Weight Loss Drugs Ozempic and Wegovy Linked to Severe Gut Problems: Study Newsweek. https://www.newsweek.com/weight-loss-drugs-ozempic-wegovy-gut-problems-health-1832375 accessed 3/19/2025
- O'Malley D. Endocrine regulation of gut function - a role for glucagon-like peptide-1 in the pathophysiology of irritable bowel syndrome. Exp Physiol. 2019 Jan;104(1):3-10. doi: 10.1113/EP087443. Epub 2018 Dec 10. PMID: 30444291.
- Funayama T, Nozu T, Ishioh M, Igarashi S, Sumi C, Saito T, Toki Y, Hatayama M, Yamamoto M, Shindo M, Tanabe H, Okumura T. Centrally administered GLP-1 analogue improves intestinal barrier function through the brain orexin and the vagal pathway in rats. Brain Res. 2023 Jun 15;1809:148371. doi: 10.1016/j.brainres.2023.148371. Epub 2023 Apr 17. PMID: 37076092.
- Holst, J. J., Andersen, D. B., & Grunddal, K. V. (2021). Actions of glucagon‐like peptide‐1 receptor ligands in the gut. British Journal of Pharmacology, 179(4), 727-742. https://doi.org/10.1111/bph.15611
- Santos-Hernández M, Amigo L, Recio I. Induction of CCK and GLP-1 release in enteroendocrine cells by egg white peptides generated during gastrointestinal digestion. Food Chem. 2020 May 30;329:127188. doi: 10.1016/j.foodchem.2020.127188. Epub ahead of print. PMID: 32516710.
- Bodnaruc AM, Prud'homme D, Blanchet R, Giroux I. Nutritional modulation of endogenous glucagon-like peptide-1 secretion: a review. Nutr Metab (Lond). 2016 Dec 9;13:92. doi: 10.1186/s12986-016-0153-3. PMID: 27990172; PMCID: PMC5148911.
- Zhu L, Huang Y, Edirisinghe I, Park E, Burton-Freeman B. Using the Avocado to Test the Satiety Effects of a Fat-Fiber Combination in Place of Carbohydrate Energy in a Breakfast Meal in Overweight and Obese Men and Women: A Randomized Clinical Trial. Nutrients. 2019 Apr 26;11(5):952. doi: 10.3390/nu11050952. PMID: 31035472; PMCID: PMC6567160.
- Hira T, Trakooncharoenvit A, Taguchi H, Hara H. Improvement of Glucose Tolerance by Food Factors Having Glucagon-Like Peptide-1 Releasing Activity. Int J Mol Sci. 2021 Jun 21;22(12):6623. doi: 10.3390/ijms22126623. PMID: 34205659; PMCID: PMC8235588.
- Indarto D, Rochmah DN, Wiboworini B, Pratama YM, Wibowo YC. Effects of Vegetables Consumption Before Carbohydrates on Blood Glucose and GLP-1 Levels Among Diabetic Patients in Indonesia. Int J Prev Med. 2022 Nov 23;13:144. doi: 10.4103/ijpvm.IJPVM_704_20. PMID: 36618536; PMCID: PMC9811965.
- Cani PD, Knauf C. A newly identified protein from Akkermansia muciniphila stimulates GLP-1 secretion. Cell Metab. 2021 Jun 1;33(6):1073-1075. doi: 10.1016/j.cmet.2021.05.004. PMID: 34077715.
Could the answer to IBS lie in the ancient practice of meditation?
IBS is a world-wide problem and the most common gastrointestinal disorder.
For a long time, irritable bowel syndrome has just been thought of as a functional problem: there’s nothing measurably, or visibly wrong with the intestines, so labeling IBS as a functional problem is almost like a shrug from the experts.
Now, IBS has earned a new classification: a disorder of gut-brain interaction. So, instead of IBS being a functional problem, there’s actually something physical that becomes disrupted – it’s just not visible to the naked eye.
What is gut-brain interaction? It is the two-way communication highway between your brain and your gut. It’s also called “gut-brain axis”. When the connection is disrupted, there are misunderstandings and overreactions that lead to IBS symptoms. You can read more about the gut-brain axis in this blog post.
What disrupts the gut-brain interaction? Many things, but a big culprit looks to be stress (1). Stress causes stress hormones to surge in the body, which turn digestion off. With a lower digestive “fire”, food digests poorly, leading to abdominal pain, diarrhea/constipation and/or bloating.
To make matters worse, the brains of people with IBS are wired in ways that make them more sensitive to stress, triggering a stress response more easily, which causes a difficult situation to turn into gut symptoms more easily as well. (2)
Solution? To mend the gut-brain interaction through stress release practices and mindset shifts.
My favorite method is meditation. It feels like an antidote to pretty much anything, sort of how exercise and good nutrition are.
When it comes to IBS, there are studies linking meditation to improved IBS symptoms, like improved abdominal pain and improved quality of life. (3)

And what I’m really excited about, is meditation’s ability to change the brain to withstand stress better (4). This means that while stress is not going to go away, you cope better with stress, and a stressful situation less easily leads to IBS symptoms. Naturally, these effects come from a long-term practice. But, even a one-time practice of a few minutes of meditation can measurably reduce stress. (5)
Personally, after 15 years of practice, daily meditation has become my secret weapon. Not only do I feel great while meditating (though not always, sometimes my brain is just too restless), I’ve noticed in general feeling calmer, more empathetic, and having a better emotional control than I used to. It feels like my brain gets triggered less easily.
One of the meditation techniques I particularly love is Hong Sau (Sau pronounced “saw”). It’s a technique of attentive focus on the breath. Since the breath is always there, it becomes an excellent object for meditation (no, meditation is not about blanking the mind). A focused mind is a calm mind, and a calm breath leads to a calm mind and vice versa. Or how do you breathe when you are reading a book with deep focus?
I’m teaching the Hong Sau meditation technique live online starting today on Wednesday January 8th 2025. There’s still time to sign up! Even if you miss the first class, you can still participate live in the remaining four. All the sessions will be recorded, so you’ll get the recording of the first session, and they will be made available for purchase as a full course after the live course is finished. Go here for more info. Sign up by emailing me at [email protected]
Questions? You got my email address.
Let’s make the year 2025 the best one yet! Let’s start by taking up meditation, or some other stress release practice, and cultivating the belief that improvement is possible – I really do believe that. Even if you feel like you’ve tried everything, something will help you, if you keep working at it.

Love,
Anna-Kaisa
References
- Cryan JF, O'Riordan KJ, Cowan CSM, Sandhu KV, Bastiaanssen TFS, Boehme M, Codagnone MG, Cussotto S, Fulling C, Golubeva AV, Guzzetta KE, Jaggar M, Long-Smith CM, Lyte JM, Martin JA, Molinero-Perez A, Moloney G, Morelli E, Morillas E, O'Connor R, Cruz-Pereira JS, Peterson VL, Rea K, Ritz NL, Sherwin E, Spichak S, Teichman EM, van de Wouw M, Ventura-Silva AP, Wallace-Fitzsimons SE, Hyland N, Clarke G, Dinan TG. The Microbiota-Gut-Brain Axis. Physiol Rev. 2019 Oct 1;99(4):1877-2013. doi: 10.1152/physrev.00018.2018. PMID: 31460832.
- Mayer EA, Ryu HJ, Bhatt RR. The neurobiology of irritable bowel syndrome. Mol Psychiatry. 2023 Apr;28(4):1451-1465. doi: 10.1038/s41380-023-01972-w. Epub 2023 Feb 2. PMID: 36732586; PMCID: PMC10208985.
- Baboș CI, Leucuța DC, Dumitrașcu DL. Meditation and Irritable Bowel Syndrome, a Systematic Review and Meta-Analysis. J Clin Med. 2022 Nov 2;11(21):6516. doi: 10.3390/jcm11216516. PMID: 36362745; PMCID: PMC9658118.
- Taren AA, Gianaros PJ, Greco CM, Lindsay EK, Fairgrieve A, Brown KW, Rosen RK, Ferris JL, Julson E, Marsland AL, Bursley JK, Ramsburg J, Creswell JD. Mindfulness meditation training alters stress-related amygdala resting state functional connectivity: a randomized controlled trial. Soc Cogn Affect Neurosci. 2015 Dec;10(12):1758-68. doi: 10.1093/scan/nsv066. Epub 2015 Jun 5. PMID: 26048176; PMCID: PMC4666115.
- Mandlik GV, Siopis G, Nguyen B, Ding D, Edwards KM. Effect of a single session of yoga and meditation on stress reactivity: A systematic review. Stress Health. 2024 Jun;40(3):e3324. doi: 10.1002/smi.3324. Epub 2023 Oct 11. PMID: 37822096.
