The gluten-free diet has become a booming trend in the recent decade. Many people follow it for perceived health benefits, like reduced inflammation. A gluten-free diet is desperately needed in the treatment of celiac disease, but what about IBS? What about health in general? Despite being trendy, is gluten-free diet a must do for good health?
Is gluten a problem for health?
Numerous studies have looked into gluten and whether restricting it might help different chronic illnesses, including IBS. Unfortunately, at the moment the evidence is clear only for celiac disease. This is the case even for inflammatory bowel diseases. There are not many studies yet, and the results in studies already done have been too variable, and many confounding factors muddle the results, which makes it difficult to say for certain that gluten is a true problem for health and gut health.
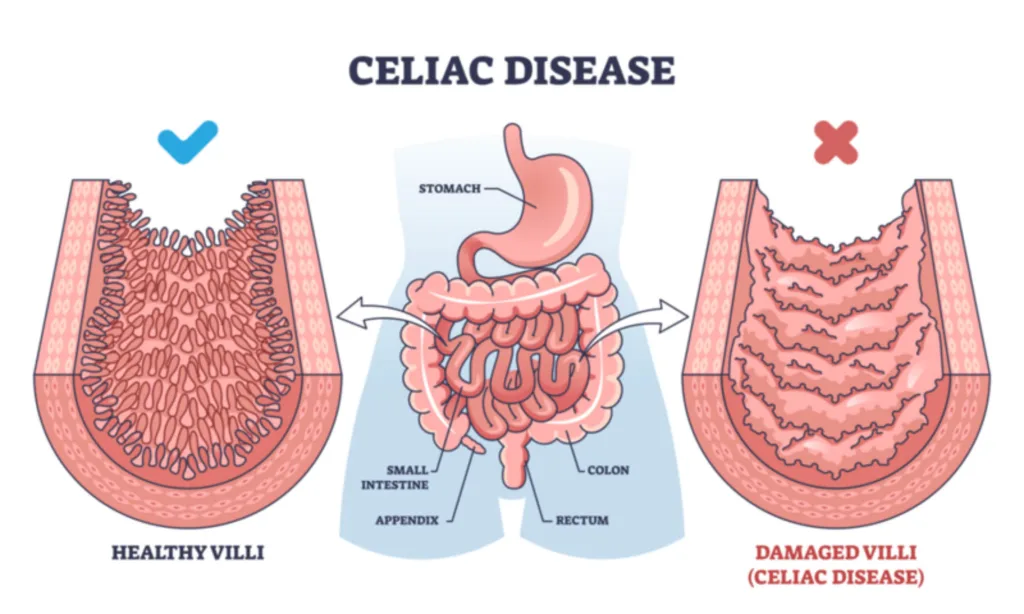
On one hand, there are studies that suggest gluten causes inflammation in the gut. It is certainly known that the severe inflammation from gluten is what causes problems in people with celiac disease and must be avoided.
On the other hand, there are numerous studies showing the anti-inflammatory effects of whole grains. The most common whole grains used in the world contain gluten, and these studies are not specifying that the grains used were gluten-free. Also, the Mediterranean diet, which favors whole grains, is considered to have anti-inflammatory effects.
Thus, it seems that gluten in whole grains does not have the same effect as gluten would on its own. It’s only in celiac disease in which the inflammatory response of the body against gluten is so strong that it overrides the anti-inflammatory effects of whole grains and can clearly be pinpointed as the problem in this illness.
It’s also worth mentioning that studies have not found that gluten causes a higher risk of weight gain, type 2 diabetes or heart disease. In fact, it’s the opposite. Eating gluten through whole grains is associated with lower weight! When the effects of fiber in whole grains are factored into the analysis, gluten on its own is linked to a lower risk of heart disease and type 2 diabetes also. The more gluten, the better it seems. Since type 2 diabetes and heart disease are associated with inflammation, the inflammatory aspect of gluten is all but clear cut.

You’d think that together with celiac disease, non-celiac gluten insensitivity (NCGS) would be an exception. In NCGS, gluten is thought to cause digestive issues without a diagnosis of celiac disease. However, what is interesting, one recent and well-executed study showed that it wasn’t the gluten ingestion, but the expectation that the food had gluten that caused symptoms to appear in people with NCGS in the study. So, if the person believed he was eating gluten, he’d get symptoms regardless of whether the food had gluten in it or not. Only a very small subset of participants seemed to genuinely react to gluten.
This phenomenon is called the placebo-effect: when you believe something helps you, or harms you, it does. Your brain and gut are intricately connected through the gut-brain axis and your thoughts and expectations have more power than you know.
So, even if it seems like gluten is problematic to you, you need to be very honest with yourself to determine whether it is the placebo effect that is responsible for your symptoms, or if it’s gluten.
Is gluten bad in IBS?
When it comes to IBS, studies have shown that other substances like fructans in gluten-containing foods are the more likely problem than gluten itself. Fructans are a type of FODMAP, which can cause gut symptoms in people who are sensitive to increased gas and/or fluid in the digestive system, which is a typical situation in IBS because of visceral hypersensitivity. Well, should you avoid gluten-containing grains because of the FODMAPs they contain then? Read this blog post to see what I think about FODMAPs.
But if gluten causes inflammation, and a lot of people feel like it causes problems, wouldn’t it be a good idea to avoid it anyway, just in case?
I have bad news for you: following a gluten-free diet might do more harm than good if you don’t have celiac disease.
Risks of a gluten-free diet
- There is evidence that avoiding gluten can be harmful to health. For one, restrictive diets in general are not great for psychological health. Fear of foods is common with restrictive diets and is mentally taxing, and difficulty finding food to eat at restaurants or at social gatherings can feel awkward and stressful. You might start avoiding these kinds of situations, which can lead to loneliness and social isolation. Mental health issues and stress often make digestive problems worse, so restricting your diet in the hopes of improving gut function can end up doing the opposite than what you were hoping for.
- Removing gluten from your diet can cause gut microbiota dysbiosis and change your gut microbiota for the worse, which has negative effects on both gut health and overall health.
- Gluten-free foods are also generally of lower quality as compared to foods that contain gluten, like whole grains. A review study revealed a significant increase in fatty liver disease and metabolic syndrome in people with celiac disease who were on a gluten-free diet and this was attributed to the fact that gluten-free foods tend to have less fiber and more sugar, salt and fat to make up for the lack of gluten. This leads to weight gain and health problems. Of course, not all gluten-containing grains are healthy either, such as packaged and highly processed foods, but whole grains that are not stripped from fiber and micronutrients are of excellent nutritional value.
- According to one study, people on the gluten-free diet had four times higher mercury levels in their body than average.
- There’s some evidence to suggest that gluten stimulates immunity. A small study saw that natural killer cell numbers were higher in the group receiving 3 grams of gluten per day than those who didn’t.

At the end, the big picture about gluten is still not completely clear – more research is needed to clarify all the contradictions. While many studies point to gluten being able to cause inflammation in the gut, it doesn’t necessarily mean that gluten is bad for you. Other studies show how gluten can reduce the risk of heart disease and diabetes, both of which are also linked to inflammation. Weird, isn’t it?
But since following a gluten-free diet is not risk-free, going on the gluten-free diet is probably not useful, and in fact, it can be harmful, if you don’t have celiac disease. If you are considering this as an option, I encourage you to discuss it with an expert so that you don’t end up harming yourself when you are trying to get better.
What I’m most interested in understanding is what are the differences between people who genuinely get symptoms from gluten and those who don’t. Or what happened that you can’t tolerate gluten anymore, even though in the past it was fine. The latter is a question I encourage you to ponder – maybe there’s something that has happened that you can reverse.
Also remember that your health and diet is never about just one nutrient or food. Whether you are healthy or not is a sum of everything you do and eat, and the effect of just one aspect of your diet might not matter as much as you might think.
Thank you for reading! If you know of people who are on the gluten-free diet, or considering it without celiac disease, share this post with them – knowledge empowers you to make informed decisions about your health. That’s why I do what I do.
References
Manza F, Lungaro L, Costanzini A, Caputo F, Volta U, De Giorgio R, Caio G. Gluten and Wheat in Women's Health: Beyond the Gut. Nutrients. 2024 Jan 22;16(2):322. doi: 10.3390/nu16020322. PMID: 38276560; PMCID: PMC10820448.
Skodje GI, Sarna VK, Minelle IH, Rolfsen KL, Muir JG, Gibson PR, Veierød MB, Henriksen C, Lundin KEA. Fructan, Rather Than Gluten, Induces Symptoms in Patients With Self-Reported Non-Celiac Gluten Sensitivity. Gastroenterology. 2018 Feb;154(3):529-539.e2. doi: 10.1053/j.gastro.2017.10.040. Epub 2017 Nov 2. PMID: 29102613.
Iven J, Geeraerts A, Vanuytsel T, Tack J, Van Oudenhove L, Biesiekierski JR. Impact of Acute and Sub-Acute Gluten Exposure on Gastrointestinal Symptoms and Psychological Responses in Non-Coeliac Gluten Sensitivity: A Randomised Crossover Study. United European Gastroenterol J. 2025 Mar 26. doi: 10.1002/ueg2.70014. Epub ahead of print. PMID: 40138597.
Algera JP, Magnusson MK, Öhman L, Störsrud S, Simrén M, Törnblom H. Randomised controlled trial: effects of gluten-free diet on symptoms and the gut microenvironment in irritable bowel syndrome. Aliment Pharmacol Ther. 2022 Nov;56(9):1318-1327. doi: 10.1111/apt.17239. Epub 2022 Sep 29. PMID: 36173041; PMCID: PMC9828804.
Cenni S, Sesenna V, Boiardi G, Casertano M, Russo G, Reginelli A, Esposito S, Strisciuglio C. The Role of Gluten in Gastrointestinal Disorders: A Review. Nutrients. 2023 Mar 27;15(7):1615. doi: 10.3390/nu15071615. PMID: 37049456; PMCID: PMC10096482.
Horiguchi N, Horiguchi H, Suzuki Y. Effect of wheat gluten hydrolysate on the immune system in healthy human subjects. Biosci Biotechnol Biochem. 2005 Dec;69(12):2445-9. doi: 10.1271/bbb.69.2445. PMID: 16377907.
Elli L, Rossi V, Conte D, Ronchi A, Tomba C, Passoni M, Bardella MT, Roncoroni L, Guzzi G. Increased Mercury Levels in Patients with Celiac Disease following a Gluten-Free Regimen. Gastroenterol Res Pract. 2015;2015:953042. doi: 10.1155/2015/953042. Epub 2015 Feb 23. PMID: 25802516; PMCID: PMC4352902.
Sanz Y. Effects of a gluten-free diet on gut microbiota and immune function in healthy adult humans. Gut Microbes. 2010 May-Jun;1(3):135-7. doi: 10.4161/gmic.1.3.11868. Epub 2010 Mar 16. PMID: 21327021; PMCID: PMC3023594.
Lebwohl B, Cao Y, Zong G, Hu FB, Green PHR, Neugut AI, Rimm EB, Sampson L, Dougherty LW, Giovannucci E, Willett WC, Sun Q, Chan AT. Long term gluten consumption in adults without celiac disease and risk of coronary heart disease: prospective cohort study. BMJ. 2017 May 2;357:j1892. doi: 10.1136/bmj.j1892. PMID: 28465308; PMCID: PMC5421459.
Michael D E Potter, Stephen C Brienesse, Marjorie M Walker, Andrew Boyle, Nicholas J Talley, Effect of the gluten‐free diet on cardiovascular risk factors in patients with coeliac disease: A systematic review, Journal of Gastroenterology and Hepatology, 33, 4, (781-791), (2018).https://doi.org/10.1111/jgh.14039
Saturni L, Ferretti G, Bacchetti T. The gluten-free diet: safety and nutritional quality. Nutrients. 2010 Jan;2(1):16-34. doi: 10.3390/nu20100016. Epub 2010 Jan 14. PMID: 22253989; PMCID: PMC3257612.
Mariani P, Viti MG, Montuori M, La Vecchia A, Cipolletta E, Calvani L, Bonamico M. The gluten-free diet: a nutritional risk factor for adolescents with celiac disease? J Pediatr Gastroenterol Nutr. 1998 Nov;27(5):519-23. doi: 10.1097/00005176-199811000-00004. PMID: 9822315.
Valvano M, Longo S, Stefanelli G, Frieri G, Viscido A, Latella G. Celiac Disease, Gluten-Free Diet, and Metabolic and Liver Disorders. Nutrients. 2020 Mar 28;12(4):940. doi: 10.3390/nu12040940. PMID: 32231050; PMCID: PMC7230624.


